UNT faculty, students and alumni are devoting their work to critical research
BY HEATHER NOEL
Medical physicist Dana Rosencranz (’98 M.S., ’02 Ph.D.) has overseen radiation for cancer patients for more than two decades, sitting alongside them as they endured their treatments. She has climbed mountains and ran 5Ks to raise funds for research, and even founded a cancer support group when she saw a need in her rural community of Paris, Texas.
But after years of helping others fight the disease that affects millions around the globe annually, the UNT physics alum received her own breast cancer diagnosis last year.
“Being a patient myself helped me gain some new perspectives,” says Rosencranz, who serves as chief medical physicist at Texas Oncology in Paris and Greenville. “We are so narrowly trained. We know our job very well, but I realized how little I knew about the other aspects of dealing with this disease. I started asking more questions than I normally would on a regular basis, and I learned so much.”
Thankfully, Rosencranz responded to treatment, but that’s not always the case.

UNT biological sciences alum Amy Schade (’13) had a good friend she thought of as a sister who died from metastatic breast cancer. It’s in her friend’s memory that Schade is working to find new treatment options for the disease as a postdoctoral research fellow at Boston-based Brigham and Women's Hospital and Harvard Medical School.
“Lexi was involved in patient advocacy through the nonprofit METAvivor. I was really inspired by her strength at the time and how she used her platform to make a difference,” Schade says. “When this job became available, it felt pretty perfect. This is something I could do to honor Lexi’s legacy by working in breast cancer.”
As the most diagnosed cancer among women in the U.S., breast cancer remains a top focus for researchers, with millions of dollars in funding allocated each year by top government agencies to learn more about the disease.
Some of that discovery is going on here at UNT and in labs and hospitals across the world occupied by members of the Mean Green Family.
During National Breast Cancer Awareness Month, learn more about the UNT faculty, students and alumni who have made it their life’s mission to further the understanding of breast cancer and are contributing to the foundational science that could lead to new treatments for the disease.
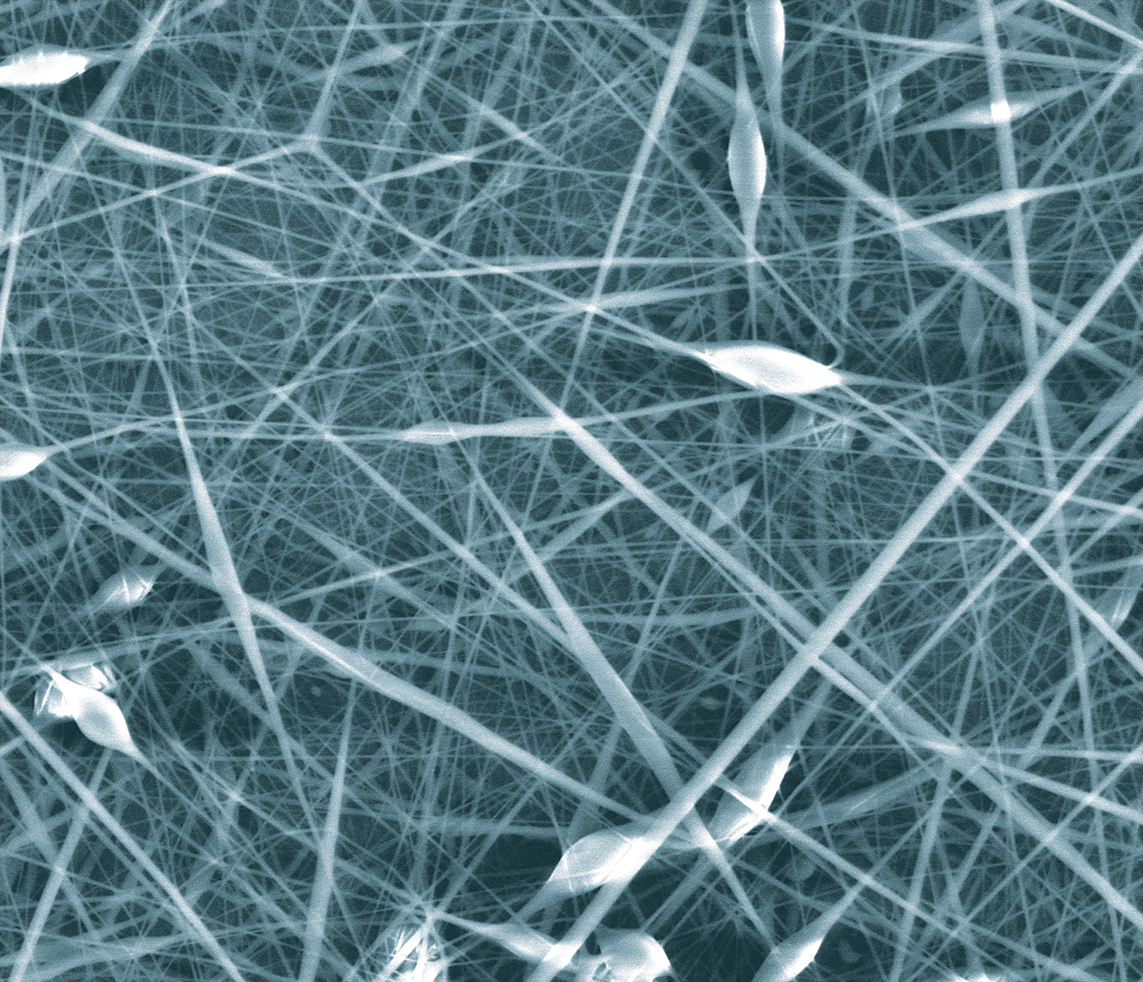
In her multidisciplinary Nanomedicine Laboratory at UNT’s Discovery Park, Neda Habibi, an assistant professor in the UNT Department of Biomedical Engineering, is exploring new therapeutic targets that could be used in the future to develop treatments for triple-negative breast cancer, or TNBC.
Following the completion of her Ph.D. in nanotechnology from the University of Genoa, Habibi found herself drawn to the application of this intricate technology in addressing critical health issues.
“Nanotechnology can be used for a lot of different industries, but I felt compelled to use this technology to address a significant health challenge like cancer,” says Habibi, who recently earned a $540,000 National Institutes of Health grant for her research. “Cancer is such a complex issue and being able to contribute to our understanding of this disease is fulfilling for me.”
Accounting for 10-15% of all breast cancer cases, TNBC is a drug-resistant type of breast cancer that does not express the estrogen receptors, progesterone receptors and human epidermal growth factor receptor 2 (HER2) protein that are seen in other types of cancers.
Rather than focusing on these cell receptors like other cancer treatments do, Habibi and her team of students are investigating an approach using self-assembling peptides — foundational ingredients of nanostructures that aid in more efficient and targeted drug delivery within the body. Specifically, they’re designing peptide substrates of the tyrosine phosphatase enzyme in TNBC that could selectively inhibit TNBC cell growth.
“Our research is looking at ways to make ‘smarter’ nanoparticles that can carry the anti-cancer drug more directly to the tumor cells for release, which could increase the drug’s effectiveness and reduce the impact on normal cells in the body,” Habibi says.
Emily Carney (’23), a doctoral student in biomedical engineering who started working in Habibi’s lab as an undergraduate this past year, is contributing to the research by preparing cell cultures for further study. Carney got into biomedical engineering through her calling to help improve people’s lives, but she’s stayed for the work she’s grown to love in the lab and the creation of new knowledge that research can bring. Thanks to the experience, she knows she’d like to establish her own lab someday.
Each weekday when Carney is taking care of her cell cultures, which she affectionately thinks of as her “babies,” she can’t help but think of her mother. Carney wonders if things would’ve been different if her mom had TNBC instead of the more treatable type of breast cancer she was diagnosed with and overcame.
“She would’ve had less resources, but the work I’m doing in Dr. Habibi’s lab could level that playing field,” Carney says. “It’s cool to be part of something that will eventually go into a publication that nobody knew before. This research could one day be a jumping off point for future scientists to create something that is a very real and helpful treatment for somebody who has breast cancer.”
Youngwook Won, UNT associate professor of biomedical engineering, is developing novel immunotherapy approaches for breast cancer in his lab. Won takes immune cells such as natural killer (NK) and T cells and arms them with more specificity and activity to target and eliminate breast cancer cells more effectively.
“These engineered immune cells can recognize and bind to specific antigens on the surface of cancer cells and trigger a cascade of events that lead to tumor cell death,” says Won, who holds 15 U.S. patents related to immunotherapy, antibody-based therapeutics, stem cell reprogramming and recombinant protein therapeutics.
The goal is to take this research and translate it into the clinical setting, where Won hopes it can make a real impact in alleviating the disease.
“My research is aimed to optimize the engineering process to minimize the potential risks and maximize the therapeutic benefits for each patient,” Won says.
While the fundamental research underway in UNT’s biomedical engineering labs is still years away from potential use with patients, Amy Schade has contributed to a new therapeutic strategy for TNBC that is in development for a Phase 1b clinical trial to test the safety, efficacy and tolerability of the treatment in people with breast cancer.
Like Carney, Schade’s first foray into research happened at UNT. She enrolled as a freshman in a course taught by biology professor Lee Hughes that gives undergraduate students the opportunity to discover new viruses as part of the UNT Phage Hunters Advancing Genomics and Evolutionary Science (PHAGES) program.
“Dr. Hughes was foundational to my understanding of the scientific method,” Schade says. “I had no concept of what real scientific research looked like before coming into his lab.”
That early interest in viruses eventually led her to studying molecular pathways and a class of viruses that cause cancer, which brought her to her current role developing novel treatments for TNBC in the lab of Karen Cichowski.

Through the research, they have identified two molecular pathways that are activated in a majority of TNBC cases and found that a combination of drugs that inhibit these pathways induces potent anti-tumor activity.
“When we use either drug as a single agent therapy, there’s almost no effect on the tumor. However, when used in combination, we now see this incredible tumor regression, reaching over 50% shrinkage after only a few days,” says Schade, who led the work and will be the first author on a pending scientific journal article on the project.
Now wrapping up her fellowship, Schade hopes to soon create her own lab where she can continue work on TNBC, including conducting further trials on the current treatment she’s studying and researching other potential therapies. In that work, she will ensure she continues to involve patient advocates like the one she’s collaborated with through METAvivor, the nonprofit her late friend volunteered with.
“Patient advocacy is a really important aspect of cancer research that’s becoming more and more valued by funding agencies,” Schade says. “As researchers, we can get wrapped up in understanding the science, but at the end of the day we’re doing all of this to improve patient outcomes and their lives.”
UNT alum Alan Prem Kumar (’93, ’98 M.S., ’03 Ph.D.) has made significant discoveries impacting breast cancer treatment as well.
Before he joined the ranks of the top 1% of most-cited scientists worldwide, Kumar was a budding researcher in biological sciences at UNT. His doctoral supervisor, the late Professor Gerard A. O’Donovan, was instrumental to his growth.
“Dr. O’Donovan encouraged us to interact with the other Ph.D. students in scientific discussions and gave all of us exposure to presenting at national conferences and writing our manuscripts,” Kumar says. “His continuous encouragement motivated us all to walk on thin ice and come out a winner. We knew we did well when he said, ‘Print ‘em, Danno.’”

Now, through his lab at the National University of Singapore, Kumar is mentoring students of his own and their work has shed valuable insight on the spread of breast and gynecological cancers, especially metastatic varieties that are considered incurable. They’ve used that knowledge for target-based precision therapies that help prevent metastasis, the spread of cancer beyond its initial site of growth in the body.
One area of growing research interest concerns Src family kinases (SFK), which are a group of enzymes in the body that are responsible for cellular responses and have been previously identified as playing a role in the transformation of healthy cells into cancer cells.
“Currently there is a lack of targeted treatments and useful biomarkers that could accurately predict the responsiveness of TNBC patients to immunotherapeutic agents and Src family kinases inhibitors,” says Kumar, who serves as a research assistant professor of pharmacology as well various leadership roles in the Yong Loo Lin School of Medicine.
Through his research, Kumar has determined that Lyn kinase is highly expressed in TNBC patients and early studies are showing promise that it could be a biological target for SFK inhibitors. Kumar’s lab is testing whether the inhibition of Lyn kinase could serve as a novel strategy to help the body’s immune system better defend against cancer and inhibit tumor progression.
Breast cancer can affect anyone, including men, but the disease is more prevalent in certain demographic groups.
For instance, the mortality rates of breast cancer are much higher for Black women, according to the American Cancer Society. When compared to white women in the U.S., Black women are 40% more likely to die from breast cancer.
While research suggests there are a variety of factors that could contribute to this inequity, UNT professor of history Constance Hilliard says the medical community is overlooking a big factor — history.
Through her study of African evolutionary history, Hilliard uncovered a link between an ethnic-specific variant of the TRPV6 gene and Black Americans’ unusually high susceptibility to a certain class of aggressive cancers, including TNBC.
“TRPV6 is predominantly found in the digestive tract because it absorbs the calcium we consume. However, it is also in the mammary and prostate glands,” Hilliard says.
The variant enables African Americans to absorb calcium at a 25-50% higher rate, which would’ve been beneficial to their African ancestors residing in lands void of cattle and therefore consuming diets low in calcium due to the absence of dairy. But in the dairy-rich lands of America, overconsumption of calcium has been identified as a trigger for certain kinds of cancer, including TNBC.
“As a historian, I’m making connections between past ecological environments' impact on people then and their ancestors today,” says Hilliard, author of the forthcoming book Ancestral Genomics: African Health in the Age of Precision Medicine from Harvard University Press. “I believe this TRPV6 gene variant is a meaningful clue that could better inform future research on breast cancer and treatment, specifically for African Americans.”
As a surgeon at UT Southwestern Medical Center in Dallas, Dr. Stephanie Serres (’06 M.S., ’09 Ph.D.) is aware of the effects breast cancer can cause. She sees patients regularly to discuss their diagnosis and treatment options and operates a few days a week on patients with high-risk breast lesions, an elevated risk of breast cancer and benign breast legions.
She says her studies in clinical psychology at UNT, coupled with her medical training, have made her specialization in breast cancer a good fit professionally.
“Breast cancer patients are a unique population that deal with a range of concerns related to their diagnosis, such as concerns of mortality, cancer recurrence, fears of impacts related to femininity, how the diagnosis will impact their role as a mother, etc.,” Serres says. “Given the complexity of the psychological overlay of their diagnosis, breast cancer was an ideal area for me to integrate my background in clinical psychology into my practice as a surgeon.”
Outside the operating room, Serres has considered a range of topics in her research, including axillary management in breast cancer patients, medicolegal issues among breast cancer surgeons, variation in care among surgical patients during COVID-19 and patient-reported outcomes. Her current research focuses on the psychological toll a breast cancer diagnosis can have on a person.
“I want to understand the diagnostic moment in breast cancer and learn how we can better interact with patients to help minimize anxiety and trauma that a patient experiences upon receipt of their diagnosis,” Serres says.
While that diagnostic moment can certainly be traumatizing for some, physics alum Dana Rosencranz felt blessed considering her job profile, giving her a knowledge advantage on top of being surrounded by qualified oncology professionals that are her friends and colleagues.
As the chief medical physicist at Texas Oncology in Paris and Greenville, it’s Rosencranz’s job to create and oversee the specialized radiation treatments prescribed by a radiation oncologist and make sure the equipment administering the radiation is working properly and meets safety standards.
Rosencranz didn’t know such a role existed growing up in Romania. She was working in cancer research when Floyd McDaniel, former UNT Regents Professor of physics, was visiting a conference in the country and suggested she come to UNT for graduate school. That recommendation ended up changing her career plans for the better. She longed to work more directly with patients and had a research interest in examining the impact of radiation on biological tissue.
“I was fortunate enough to literally stumble over this world of medical physics,” Rosencranz says. “Some people don’t even know that cancer is treated with radiation or that there is a physicist that creates and checks everything before they get to the radiation machine for treatment.”
Going through her cancer journey has enabled her to gain more understanding from the patient perspective. It’s insight she can now pull from if patients come in with questions about other parts of cancer care.
“If they have technical questions about radiation, I can certainly provide them with those answers, but now going through my own cancer, I also think of my role with patients as being someone who can bring hope,” Rosencranz says. “I want people to know my heart and encourage them that they can get through this challenge.”

